Anthony Siino considers himself to be a levelheaded person, and as director of regulatory affairs for biologics at Pfizer, one of the largest pharma companies in the world, he has to be. But when a visit to the doctor in October 2016 turned into a diagnosis of hepatocellular carcinoma — or a liver cancer — his normally calm demeanor instantly changed.
“I never get frazzled,” he says. “And I was frazzled. I was thinking a thousand miles an hour.”
Siino went from doctor to doctor, confused. Eventually, he reached out to Susan Harabedian, a physician’s assistant at Pfizer’s corporate office in Peapack, New Jersey. Harabedian liaised with HR and recommended Siino get in touch with PinnacleCare, a health advisory service that Pfizer offers as a benefit to employees who are diagnosed with serious diseases to help them better navigate their care.
“They like the benefits they work on diligently to be used,” Harabedian says of Pfizer’s HR team.
Pfizer
Much like a football team, every huddle has a “quarterback” who coordinates communication between all of the members and makes sure the employee’s interests are the first priority. The company also has a cancer huddle playbook, a document that provides information on the huddle and the company’s benefits.
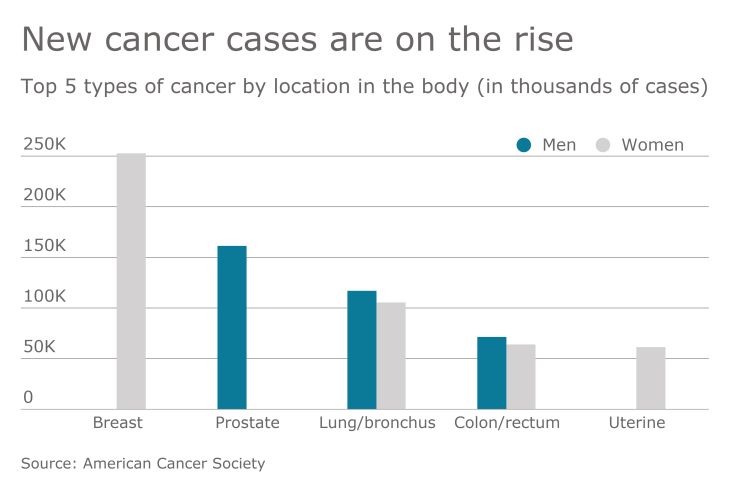
“Cancer is significant. It’s been our top medical conditions for the past several years — we see it not only on the medical claims side but on the disability side as well,” says Michele Proscia, director of U.S. health and insurance benefits and policy at Pfizer. “We know that it has a significant impact on our colleagues, whether they’re the member going through the cancer treatment or they’re supporting a family member or loved one with cancer.”
Pfizer would not comment on the number of employees that have been in the cancer care huddle or the number of employees who have used PinnacleCare.
The huddle of Pfizer’s vendors meets about twice a month to make sure they are providing employees the best possible care. The company also is putting together an onboarding kit for new benefits vendors to be added in the future, Proscia says.

Podcast:
“It’s important to engage our vendors throughout the process,” Proscia says. “We wanted our vendors to understand how these different organizations work together.”
It’s unclear if other companies have developed a cancer care benefits program that is as comprehensive as Pfizer. The pharma company worked with the Northeast Business Group on Health in the initial development of the cancer care huddle program. Candice Sherman, CEO of NEBGH, says to their knowledge Pfizer has been on the “forefront of developing and implementing this type of model” but other companies may take similar approaches.
“I think it’s fair to say that other companies have brought vendors together to better coordinate benefits and services,” Sherman adds. “We hope that the guide NEBGH put together will help other companies think about how a huddle or similar concept might work for them when it comes to cancer care for their employees.”
Pfizer brought together all of its healthcare benefit vendors for a summit in July 2017, says Dr. Miles Varn, chief medical officer at PinnacleCare. Varn says the summit was an opportunity to meet with others involved in the huddle to get a better sense of how they could individually help the patient.
“They brought everyone together in the same room, so their other vendors would have a specific understanding of where we would be helpful for the patient,” he says.
Brenna Shebel, vice president of the National Business Group on Health, says companies that provide a second-opinion service and cancer huddle to employees are on the “forefront” of cancer benefits. Cancer is a difficult disease to navigate, she says, as treatment plans can vary greatly by type.
“Companies that bring in outside groups are really forward-thinking as far as supporting employees with a diagnosis,” Shebel says.
Cancer huddles can also mean employees are able to get access to better treatment. When Siino was first diagnosed, for instance, the doctors he went to recommended he get a liver transplant. But when he began working with PinnacleCare, they told him to get a second opinion from a specialist in liver cancer — something he may not have been able to do on his own.
Telemedicine, employee assistance programs and nutrition counseling are among the offerings that have increased in popularity, according to a new report from Korn Ferry and WorldatWork.
The service referred Siino to a surgeon who specializes in liver cancer and recommended he have another procedure, called a liver resection, which removes the cancerous part of the liver instead of the entire organ. Siino agreed, and he had the procedure in January 2017. It was successful, and so far, Siino has had no recurrence of cancer.
“They were able to get me the best of the best,” Siino says. Varn says there are benefits for patients, particularly those diagnosed with cancer, to getting a second-opinion from a doctor at a research hospital, where scientists actively study a disease. Varn explains that doctors at research hospitals are typically more specialized than those at local hospitals and tend to be more aware of the most recent research on a particular kind of cancer.
“We’re looking to set them up with an expert for their particular problem,” Varn says.
But Pfizer is unique. While some companies have made improvements to their cancer benefits over the years, the offerings
Plus, employers often have an extra challenge: Employees don’t always listen to or understand their benefits until they have to. HR might inform workers about cancer benefits during open enrollment, but unless a worker receives a cancer diagnosis, they generally pay little attention, Shebel says.
Shebel says a strong employee network can help increase the likelihood that workers will know about and therefore use their cancer benefit offerings. For example, when Siino discovered his colleague’s son had been diagnosed with cancer and was having trouble getting an appointment with a specialist, he shared his experience and recommended he reach out to PinnacleCare.
Although Siino is no longer actively using PinnacleCare and the company’s other cancer care benefits, he still tries to share information about them whenever he can. He doesn’t think enough people at the company know about the offerings.
“This stupid disease is becoming more prevalent,” Siino says. “When you have a resource like that, it is such a benefit.”






