Mental health support is becoming a top concern for employers as more workers struggle with increased anxiety, loneliness and depression related to remote work during the coronavirus pandemic.
Some 56% of employees said they had experienced increased anxiety due to working from home and social distancing. Fifty-three percent said they had experienced increased loneliness and 53% reported their productivity levels had been negatively affected, according to a new study by Blind, an anonymous professional network.
“We’re facing a time of uncertainty — not just with coronavirus but with the things that attach themselves to that,” said Jerrod Helms, vice president and head of sales at
Left without the option of visiting a primary care physician — who are often the first to diagnose signs of stress or mental illness — employees are falling through the cracks in getting the care they need. On average, just half of people dealing with mental health or stress-related issues actually receive treatment, according to the National Alliance on Mental Illness.
Read more:
Often, employees don’t have access to healthcare plans that integrate behavioral health solutions into more traditional healthcare models, said Dana Udall, the chief clinical officer at Ginger.
“There are solutions and some of them are good, but typically, they’re only meeting the needs of a small segment of the population,” Udall says. “They’re not part of a system that allows people to get collaborative treatment from different providers.”
While employers have addressed mental health needs through app-based platforms, EAPs and telehealth offerings, these services are often treated as add-ons to existing health plans. Programs that focus just on building a mindfulness practice, for example, don’t boost engagement and there’s no accountability for employees to participate and see changes, Udall said.
Other solutions, like therapy or psychiatry network extenders, create “ghost networks because there’s limited availability and they don’t take insurance,” she said. And if an employee is able to connect with a therapist, coverage may only be covered for a short amount of time.
“It’s hard to tell if care is effective,” Udall said. “It's an abrupt experience if you're in therapy for 8 weeks and suddenly that's pulled away.
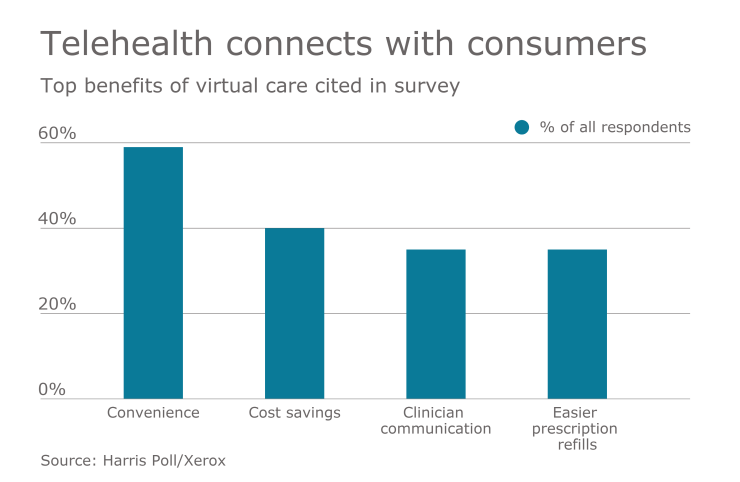
Instead, employers should be tapping into programs that address a full spectrum of need, utilizing technology to address and overcome common roadblocks around getting care, like stigma, accessibility and cost, Helms said.
“What we’re seeing leading edge companies do is invest in an effective healthcare system built around allowing everyone to have access to care at any time,” he says. “Artificial intelligence, when married to a care team to deliver care and support, is that much more effective, and delivered 24 hours a day.”