With thousands of insurance brokers and consultants for employers to choose from, deciding on a new adviser can be overwhelming. For industry producers, it’s easy to get lost in a densely wooded forest of choices.
But this decision is so critically important — and it can have significantly more impact on the cost and quality of a full benefits plan than the insurance carrier itself.
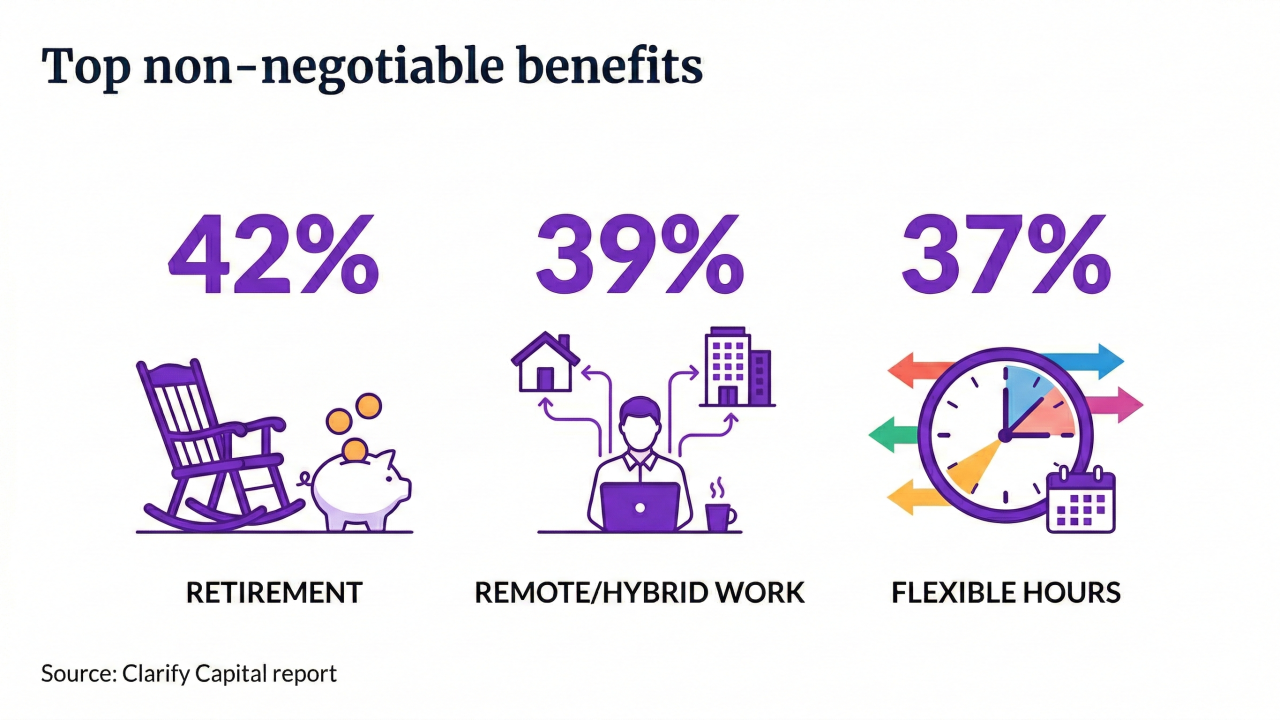
Selecting the right benefits package and best health insurance plan are decisions that must be made carefully to ensure employee satisfaction and to remain competitive in hiring, with a focus on cost. For employers, the path throughout a buyer’s journey can feel convoluted and complex. To forge an easier way forward, I encourage employers in the process of researching and evaluating brokers to exercise caution.
Read more:
Here are four red flags for employers to watch for when selecting a new insurance broker, which can also be used as a yardstick — or reality check — by which brokers can measure whether or not their work will help them stand out from the pack.
Hesitation when asked about comparable-size clients.
Each industry and employer-size group has its own unique strategies and tactics to offer comprehensive benefits at competitive costs, and these strategies evolve each year. A midsize transportation company has different needs than a large regional law firm; that variance spans from health insurance across life, disability, leave and retirement.
You would not visit a cardiologist if you were experiencing knee pain — and in the same way, it’s imperative that the insurance adviser under consideration has demonstrated experience with similar employer groups. The broker or consultant should be able to walk the prospect through comparable clients and strategies they deployed.
Read more:
If the broker struggles to source examples or provide data that supports their claim, that’s a red flag. You don’t want to be an orthopedic surgeon’s first surgery. Employers will not want to hand their benefits to someone without any experience around their specific needs.
Their pitch is too good to be true.
If the new plan seems too good to be true, then chances are that’s exactly the case. This is a good tactic to generate meetings and interest, but be wary. If presented with a new plan that can save you 25% a year, there is a downside somewhere — if you squeeze one side of the balloon, it pops out the other side.
Massive cost decreases equate to limited networks, aggressive utilization strategies and provider payment tactics rife with friction. Thoughtful employers will do their own research, including asking to speak with current clients they have in that plan. It’s important to understand what turnover rates look like with participants in that plan after year two and three. It certainly helps to have been in the industry long enough to know when something doesn't feel right. Trust your gut.
Failure to supply independent market data to support benefit plan recommendations.
There are more than 10 million employers in the U.S., which means there are likely others just like the one shopping for a new broker. Does the insurance adviser provide independent benchmarking with comparable companies to help guide the prospective buyer’s plan design?
Read more:
Independent data is important. Otherwise, it's like a car dealership using its own data to support pricing. People use data to drive their decision-making in every other facet of life, and it should be a priority here, too.This includes referencing ratings and reviews from other brokers of the insurance company and adviser under consideration.
Lack of transparency on fees and commissions.
Employee benefits and health insurance plans are big investments. For this reason, all line items, additional fees and coverage terms should be easily laid out in a simple format to review.
There should be no hesitation to ask about a broker’s fees and commission, or reluctance on the part of that producer to provide such information. If there’s no willingness to be transparent, then it’s reasonable to expect the prospective buyer will continue researching and interviewing other brokers. Fee transparency should be expected in all aspects, from medical benefits to ancillary products and services such as human resource information systems, third-party administrators, telehealth services and vendor products.
It’s also important to ask PE/PM questions and inquire about one-time payments. Brokers should be paid for support across all services; it is a highly valued consulting skill set that adds direct value — but that payment needs to be transparent to all parties for the benefit of the broker and client.
Read more:
Deciding to retain or change an insurance adviser can prove challenging, but it’s a step that must be assessed just as critically as any other major business decision. That means researching and vetting potential candidates; interviewing and asking for references; evaluating and comparing plans against one another.