For employers struggling to manage healthcare costs because of exorbitant third party administrative costs, a new partnership will create more ease and cost savings.
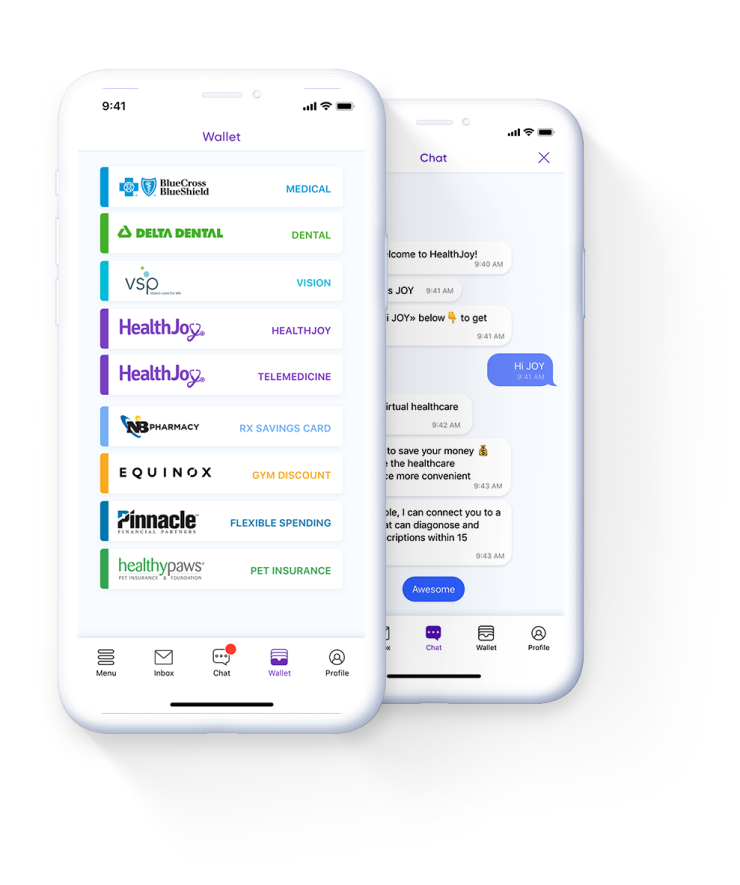
Benefits platform HealthJoy has teamed up with Auxiant, an interactive web based application that provides access to health plan information on a 24/7-basis, to debut a new product called HealthJoy TPA+. The partnership allows HealthJoy to tap into Auxiant’s claims and data to enhance its virtual assistants, which will help their employer and consumer clients make better choices regarding healthcare decisions, while containing costs.
“Technology starts with data to create the right kind of digital experience and to make that experience meaningful,” says Chad McMahon, director of TPA partnerships at HealthJoy. “The TPA partnership gives us access to data events around when providers verify insurance for members.”
Before an employee even gets to see a doctor, that office will verify their insurance through the Auxiant partnership. HealthJoy has daily access to this information, and also receives precertification information daily. Additionally, insurance claim data is accessed on a monthly basis.
This broad and in-depth access allows HealthJoy to personalize the healthcare experience for their clients, McMahon says.
“Each of those data sets will tell us when a person is using the healthcare system so that we know when to proactively reach out to them and provide a more real-time experience,” he says. “As you get into the precertification claims data, there’s information in those data sets that tell us what a member is going through. We can really start to personalize, and that puts us in a position to pre-populate guidance to that member.”
By utilizing the data Auxiant provides, HealthJoy will be able to enhance its AI-powered virtual assistant and concierge team so they can proactively assist members in their healthcare journey. Employees will get better quality care at a fair price, saving money for both employees and their employers.
“As we really started to get deeper and more integrated into the benefits space, we realized that there was a huge opportunity if we started to look at strategic partnerships that allow us to extend further back into the care delivery process to create a more integrated and valuable experience from the benefits side of things,” McMahon says.
There are
When HealthJoy first examined where it could make the biggest impact, third party administrators seemed to be the most obvious starting point because they are the centerpiece from where all the data claims flow.
“This partnership gives us a huge opportunity to create a better member experience and it opens up a lot of avenues as we move forward and continue to iterate on what this product is and what else we can bundle into it,” McMahon says.
Data is critical in providing a positive healthcare experience for employees, says Joe Holt, vice president of sales and marketing for Auxiant. A TPA is a valuable asset when understanding how to properly utilize it.
“We saw this as the perfect opportunity to share data in a meaningful way,” Holt says. “Being proactive with claims and pre-certification data is a game-changer for the TPA space.”