You’ve likely heard something about accountable care organizations, which help to lower healthcare costs by shifting the focus from fee-for-service payments to outcomes-based payments.
ACOs are groups of physicians, hospitals, nurses and other care providers who agree to be accountable for the care they provide, as well as patient outcomes and the total cost of care. Providers in an ACO work closely together to ensure that patients get the care they need in a seamless way that focuses on quality, rather than volume.
Maybe you’re wondering if an ACO is the right solution for your organization. Before considering that, it’s helpful to look at how we got to this point in health insurance.
The 1920s first brought the idea of health insurance to consumers in the form of pre-paid hospital services from individual hospitals.
Then, during World War II, the federal government implemented wage controls, forcing employers to develop more creative strategies for attracting workers. Demand for employees was up, but the controls prohibited companies from paying people more. Health insurance and sick leave didn’t count as wages, and thus, employer-sponsored health insurance was born.
Since then, healthcare spending has increased — at a moderate rate decade over decade until 2000, when spending began increasing by double digits each year, according to the Kaiser Family Foundation.
In 2012, the U.S. spent more per person than other nations, though our overall healthcare performance ranked 37 out of 191 countries, according to the World Health Organization. These increasing costs have become a burden for both companies and consumers. It became more common for consumers to cut pills in half, postpone care and stop refilling prescriptions
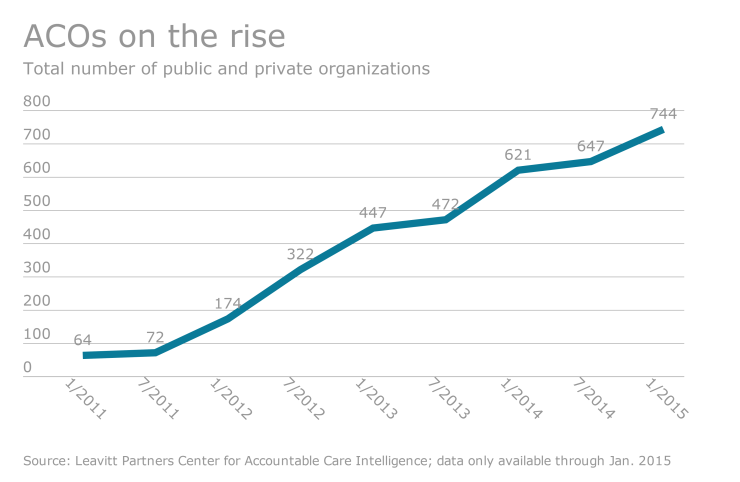
These ongoing cost increases mean that employers are now focusing on cost-containment measures to try to keep their fees — and the fees employees must pay — down. In recent years, that has led to the rise of ACOs. ACOs are helping some employers keep costs from continuing to grow steeply — and they might help employees stay healthier, too.
The federal government developed the framework for ACOs in the early 2000s. When the Affordable Care Act was first being implemented, the Centers for Medicare and Medicaid backed the concept of ACOs. Private physician groups and hospitals soon followed.
In the usual scenario, a consumer might search for a physician through her network portal and find a doctor based on whether or not they’re taking new patients, the specific location of the office and the overall convenience of that provider. Consumers typically have access to hundreds of doctors whose quality of care can vary greatly, and who are compensated on a fee-for-service basis.
An ACO ensures that each patient gets the best care possible and is seen by providers who are motivated by patient outcomes, rather than volume. This also means providers in an ACO work closely together across the continuum of care to ensure that patients get the right high-quality care from the right provider at the right time. The arrangement decreases the chance that a patient will have duplicate tests done or have access to multiple prescriptions from different doctors.
It also increases the chances that a patient who has a major surgical operation such as a hip replacement, for example, will be prescribed the minimum amount of pain medication, complete rehabilitation, get follow-up care as needed and return to work after a speedy recovery — all without a return trip to the hospital.
Additionally, an ACO arrangement requires providers to closely manage patients with chronic conditions.
In addition to helping employers control health spend because of improved care coordination and a focus on outcomes, ACOs can also create a more direct relationship between employers and providers — and more opportunities to control costs. Employers are able to look at how providers care for patients and what types of medicines they’re prescribing. With this information they may be able to better manage the types of care patients receive that greatly affect medical spend or long-term patient outcomes.
When the pieces are in place — providers shift the way they care for patients, use technology to coordinate care and successfully meet quality goals — ACOs can limit cost growth year over year while providing the right care at the right time. As best practices are developed, payment policies mature and current ACOs renew their contracts, we’ll continue to see growth in this model of care.